If you're 44 or older, your brain networks are already destabilizing. Not from lost neurons. Not from plaques or tangles. From metabolic stress—specifically, your neurons' declining ability to use glucose for fuel.
This isn't speculation. A 2020 study from Stony Brook University analyzed brain network stability in over 19,300 people and found a sharp transition at age 44. Before that point, brain networks are remarkably stable. After 44, they begin to fragment. By 67, the deterioration accelerates dramatically (Mujica-Parodi et al., 2020, PNAS).
The culprit: Neuronal insulin resistance—your brain cells losing the ability to import glucose despite normal blood sugar levels. It's "type 3 diabetes," brain-specific, and it can happen even if your body's metabolism is perfect.
The metabolic dysfunction begins decades before cognitive symptoms appear. By the time someone struggles with memory in their 70s, they've been metabolically compromised since their 40s.
But here's the opportunity: The study found a critical intervention window (ages 40-59) when metabolic support can stabilize brain networks. After 60, the window starts closing—vascular damage and neuronal death become irreversible.
This article breaks down the mechanism, the timeline, and what you can do about it. If you're in your 40s or 50s, pay attention. This is your window.
The S-Curve of Brain Aging (It's Not Gradual—It's Punctuated)
For decades, we assumed brain aging was linear: slow, steady decline from 20 onward. Wrong.
The Stony Brook study analyzed functional connectivity—how well different brain regions communicate—across 19,300+ individuals. They found brain aging follows an S-shaped curve with three distinct transitions:
Transition 1: Age 44 (The Bend Before the Break)
What happens:
- GLUT4 glucose transporters in neurons become insulin-resistant
- Connections between regions weaken
- Metabolic stress becomes measurable on fMRI
- But: Cognitive function still appears normal (compensation is working)
Why you don't notice: Your brain compensates by recruiting additional regions, shifting metabolic processes, upregulating backup systems. Tests of memory and attention look fine. But beneath the surface, your neurons are working with diminishing energy.
It's like a business running on dwindling cash reserves. Operations look normal from the outside, but the balance sheet is deteriorating.
Transition 2: Age 60-67 (Rapid Acceleration)
What happens:
- Network deterioration accelerates dramatically
- Vascular effects compound (small vessel disease, white matter lesions)
- Compensation starts failing
- Cognitive symptoms emerge (memory lapses, slower processing, word-finding difficulties)
Why it suddenly feels "rapid": It's not. The underlying issues have been building for 15-20 years. What's rapid is the failure of compensation. Once the system can't keep up, decline becomes obvious.
A dam with a slow leak. For years, you patch it and it holds. Then one day, the patches fail and the whole thing collapses.
Transition 3: Age 90+ (Plateau)
What happens:
- Deterioration slows (paradoxically)
- Likely because the most vulnerable neurons have already died
- Survivors are more resilient
Clinical note: This plateau is not "recovery"—it's the exhaustion of vulnerable neurons.
The Mechanism: Neuronal Insulin Resistance (Why Your Brain Can't Use Glucose)
Your Brain's Energy Demands
Your brain is metabolically expensive:
- 2% of body weight
- 20% of body's energy consumption
- ~120g of glucose per day (equivalent to 480 calories)
Most of this energy comes from glucose. But glucose can't just diffuse into neurons—it needs a transporter.
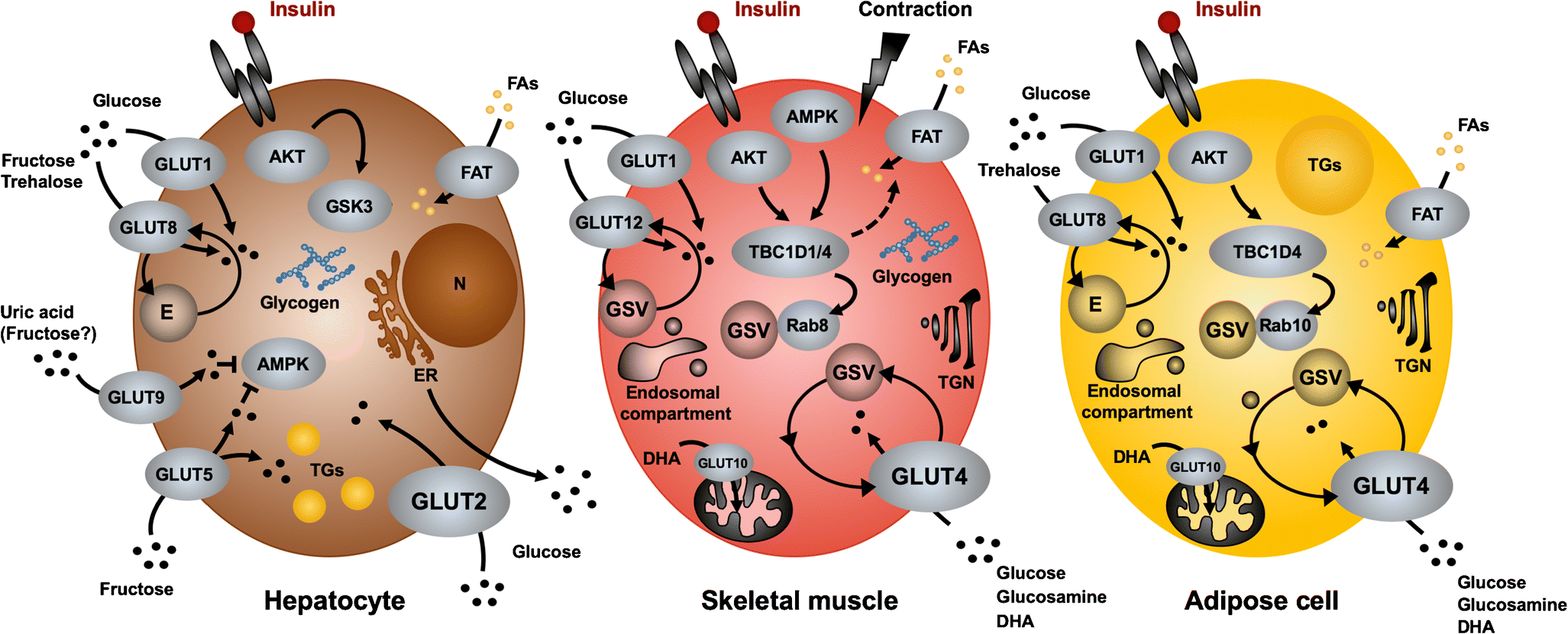
The GLUT4 System (And Why It Fails)
Normal glucose metabolism:
- Glucose in bloodstream
- Insulin signals neurons: "Energy available"
- Neurons move GLUT4 transporters to cell membrane
- Glucose enters → glycolysis → Krebs cycle → ATP (energy)
In neuronal insulin resistance:
- Glucose is present (blood sugar is normal)
- Insulin is present (may even be elevated)
- GLUT4 response is blunted → glucose can't enter neurons
- Neurons are energy-starved despite being surrounded by fuel
This is not the same as type 2 diabetes. You can have perfect blood sugar, no metabolic syndrome, healthy weight—and still develop neuronal insulin resistance. The brain's insulin signaling operates semi-independently.
Why Age 44?
Starting at age 44, neurons lose oscillatory insulin signaling patterns. This creates a cascade: brain cells cannot effectively utilize available glucose, extracellular sugar accumulates, glycation (tissue 'rusting') accelerates, inflammatory processes increase, and neural connectivity degrades.
Proposed mechanisms:
- Cumulative oxidative stress: Decades of reactive oxygen species (ROS) damage insulin receptors
- Chronic inflammation: Low-grade systemic inflammation impairs insulin signaling
- Mitochondrial decline: Aging mitochondria produce less ATP, creating feedback loop
- Insulin receptor downregulation: Years of high-carb diet may desensitize receptors
The data:
- Metabolic changes precede vascular changes (they're not parallel processes)
- Brain glucose hypometabolism is detectable 10-20 years before Alzheimer's diagnosis (Cunnane et al., 2016, Journal of Alzheimer's Disease)
- APOE ε4 carriers (Alzheimer's risk gene) show worse insulin resistance effects
Neuronal insulin resistance is upstream of the pathology. Amyloid plaques, tau tangles, vascular damage—these are consequences, not causes.
The Compensation Phase (Ages 44-60)
Why don't you notice cognitive decline in your 40s and 50s? Compensation:
Neuroplastic strategies:
- Recruiting additional brain regions to complete tasks (bilateral activation instead of unilateral)
- Shifting metabolic pathways (relying more on lactate, astrocyte support)
- Increasing synaptic strength to compensate for fewer functional neurons
The problem:
Compensation is metabolically expensive. It works temporarily, but it's not sustainable. By your 60s, the compensation system itself starts failing.
Clinical implication:
Normal cognitive tests in your 50s don't mean your brain is healthy—they mean it's compensating well for now. The underlying stress is real.
The Ketone Solution: An Alternative Fuel That Bypasses Insulin
When researchers discovered neuronal insulin resistance, they looked for solutions. The answer was already in your metabolic toolkit: ketones.
How Ketones Work (The MCT2 Bypass)
Ketones (beta-hydroxybutyrate, acetoacetate) are produced when you:
- Fast for 12+ hours
- Follow a ketogenic diet (<50g carbs/day)
- Take exogenous ketone supplements
- Exercise intensely (mild ketosis)
The key difference from glucose:
Glucose pathway:
- Glucose → GLUT4 (insulin-dependent) → glycolysis → Krebs cycle → ATP
Ketone pathway:
- Ketones → MCT2 transporters (insulin-independent) → acetyl-CoA → Krebs cycle → ATP
MCT2 doesn't require insulin. It's an express lane that bypasses the traffic jam. Once inside, ketones feed directly into the Krebs cycle, producing ATP just as effectively as glucose.
The Intervention Study: Ketones Stabilize Brain Networks
Mujica-Parodi's team tested this directly. They gave 101 participants ketone drinks and measured brain network stability with fMRI.
Results:
- Ketones significantly stabilized brain networks
- Effect was strongest in ages 40-59 (the critical window)
- Glucose supplementation had no effect (makes sense—the problem is insulin resistance, not glucose availability)
Age-specific effects:
| Age Group | Brain State | Ketone Response | |-----------|-------------|-----------------| | 20-39 | Stable, pre-destabilization | Minimal benefit (networks already stable) | | 40-59 | Metabolic stress, still viable neurons | Maximum benefit ← Critical window | | 60-79 | Vascular damage, some neuronal death | Diminished benefit (too late for many neurons) | | 90+ | Severe decline | Not studied (likely minimal effect) |
The takeaway:
Ketones can "rescue" metabolically stressed neurons, but they can't resurrect dead ones. You need to intervene while neurons are struggling but viable.
The Critical Intervention Window (Ages 40-59): Why Timing Is Everything
This is the core finding: Metabolic interventions work best before symptoms appear, during the "bend before the break" phase (ages 40-59).
Why Waiting for Symptoms Is Too Late
In your 40s-50s:
- Neurons are metabolically stressed
- But they're still alive, still functional
- Compensation is working
- Intervention can stabilize them
In your 60s-70s:
- Years of energy starvation have triggered cascades:
- Endothelial dysfunction (small vessel disease)
- Amyloid accumulation (impaired clearance)
- Neuroinflammation (microglia activation)
- Neuronal death (apoptosis)
- Some of this is irreversible
- Intervention is less effective
Why Alzheimer's drug trials fail:
Most enroll people in their 60s-70s with symptoms. By then, you're trying to rescue neurons that are already dead. The metabolic damage happened 15-20 years earlier.
Don't wait for memory problems. Start metabolic support in your 40s, when neurons are stressed but salvageable.
Practical Strategies for the 40-59 Age Group
If you're in the critical window, here's what the science supports:
Strategy 1: Periodic Ketosis
Goal: Give your brain regular access to ketone fuel without requiring permanent dietary restriction.
Options:
- Intermittent fasting (16:8): Fast 16 hours, eat in 8-hour window. Mild ketosis after 12-14 hours.
- Weekly 24-36 hour fast: Once a week, skip dinner through next day's lunch. Deeper ketosis.
- Ketogenic diet (periodic): 1-2 weeks per quarter on strict keto (<50g carbs/day). Resets metabolism.
- Exogenous ketones: Ketone esters or salts on non-fasting days. Rapid ketosis (30-60 min).
Start here: 16:8 intermittent fasting, 5 days/week. It's the easiest entry point.
Strategy 2: Exercise (The Insulin Sensitizer)
Mechanism: Exercise improves neuronal insulin sensitivity via:
- AMPK activation (metabolic sensor that upregulates glucose transporters)
- Reduced inflammation (lowers inflammatory interference with insulin signaling)
- Increased BDNF (promotes neuronal health and metabolic function)
- Mild ketosis during prolonged aerobic exercise
Protocol:
- Aerobic: 30-60 min, 4-5x/week (Zone 2 intensity—conversational pace)
- Strength: 2-3x/week (muscle mass preserves metabolic health)
- HIIT: 1-2x/week (maximal AMPK activation)
Evidence: Aerobic exercise improves glucose metabolism in aging brains (Erickson et al., 2011, Hippocampus). It's probably the single most effective intervention for neuronal insulin sensitivity.
Strategy 3: Sleep Optimization
Why: Sleep deprivation impairs glucose metabolism globally—including in the brain. One night of poor sleep reduces insulin sensitivity by 20-30%.
Protocol:
- Consistent wake time (7 days/week)
- 7-9 hours total sleep
- Prioritize deep sleep (first 3-4 hours of night)
Track with Oura Ring, Whoop, or simple sleep diary.
Strategy 4: Anti-Inflammatory Diet
Why: Chronic inflammation impairs insulin signaling. Reducing systemic inflammation helps preserve neuronal insulin sensitivity.
Protocol:
- Mediterranean diet (fish, olive oil, vegetables, nuts, berries)
- Omega-3s: 1-2g EPA+DHA daily (fish or supplements)
- Minimize ultra-processed foods, refined carbs, seed oils
- Polyphenols: Coffee, green tea, dark chocolate
Evidence: Mediterranean diet reduces Alzheimer's risk by ~30-40% (Scarmeas et al., 2009, Annals of Neurology). Mechanism likely includes improved insulin sensitivity.
Strategy 5: Monitoring
You can't manage what you don't measure.
Biomarkers:
- Fasting glucose (<100 mg/dL)
- Fasting insulin (<10 µIU/mL; lower is better for brain health)
- HOMA-IR (<2.0; measures insulin resistance)
- HbA1c (<5.7%)
Cognitive tracking:
- Annual cognitive testing (MoCA, Trail Making Test)
- Establish baseline in your 40s, track changes
Brain imaging (optional but powerful):
- MRI with volumetric analysis (hippocampus, cortical thickness)
- fMRI resting-state (network connectivity)
- PET with FDG tracer (brain glucose metabolism)
The APOE Wild Card
APOE ε4 is the strongest genetic risk factor for Alzheimer's (3-15x increased risk for homozygotes).
How it relates to insulin resistance:
APOE is a lipid transport protein. The ε4 variant impairs lipid metabolism and worsens the effects of insulin resistance. It's a metabolic double-whammy.
Implications:
- If you're APOE ε4+, metabolic interventions are even more critical
- Ketones may be especially beneficial (Henderson et al., 2009, Alzheimer's & Dementia showed cognitive improvement in ε4+ MCI patients with ketone esters)
- Exercise and fasting become non-negotiable
Should you get tested?
Controversial. Knowing you're ε4+ doesn't change the interventions (they're the same), but it might increase motivation. 23andMe reports APOE status.
Brain Wave Slowing: Your EEG as a Dementia Biomarker
Beyond metabolism, there's another measurable marker of brain aging: Individual Alpha Frequency (IAF)—the peak of your alpha brain wave rhythm.
The IAF-Age Trajectory
Normal decline:
- Young adults: 10-11 Hz
- Middle age: 9.5-10 Hz
- Elderly: 8-9 Hz
- MCI/early dementia: <8 Hz
IAF <9 Hz = high dementia risk. This is one of the most reliable EEG predictors of cognitive decline—more sensitive than many cognitive tests. It reflects "thalamic clock speed"—how fast your brain can process information.
Why IAF Slows With Aging
Metabolic basis:
- Neurons running on less glucose → slower firing rates
- Reduced mitochondrial function → lower energy availability
- Thalamocortical circuits become "sluggish"
IAF slowing parallels the metabolic decline we've been discussing. It's a functional readout of the energy crisis in your neurons.
IAF as an Early Warning System
The advantage: IAF can be measured with QEEG in a clinical setting. If your IAF is slowing (especially <9.5 Hz in your 40s-50s), it's a red flag for:
- Neuronal insulin resistance
- Impending cognitive decline
- Need for aggressive metabolic intervention
IAF slowing can be detected before cognitive symptoms emerge. It's a leading indicator, not a lagging one.
Can You Train IAF Back Up?
Yes—neurofeedback can increase IAF.
The PAF+1 Protocol:
- Measure your baseline IAF (e.g., 8.5 Hz)
- Train at your upper alpha edge: IAF to IAF+2 Hz (e.g., 8.5-10.5 Hz)
- This "pulls" the peak frequency upward over sessions
Dose for aging brains:
- 30+ sessions minimum (older brains require higher doses due to reduced plasticity)
- 2-3x per week
- 30-45 min per session
- Total: >300 min training time (meta-analysis threshold for memory effects)
The paradox:
- IAF increase is transient: Returns to baseline within 30 days post-training
- BUT cognitive gains persist 1-12 months: Memory improves, processing speed increases, executive function sharpens
Training at the upper alpha edge repeatedly recruits faster thalamocortical circuits, strengthening connectivity and network efficiency. Even when frequency reverts, the improved network function remains—like building muscle strength that persists even when you stop lifting as frequently.
IAF Training as Metabolic Support
The connection to ketones/fasting:
- Neurofeedback trains network efficiency (top-down)
- Ketones/fasting provide metabolic fuel (bottom-up)
- Combining them likely synergizes
If your IAF is <9 Hz, consider:
- Start metabolic interventions (ketones, fasting, exercise)
- Add IAF neurofeedback (30+ sessions)
- Re-measure IAF every 6-12 months to track trajectory
- Continue maintenance neurofeedback (quarterly boosters) if IAF drifts back down
Clinical note: IAF training works best before advanced neurodegeneration. If you're in the critical window (40-60), this is high-value intervention.
Brain Waves + Metabolism = Comprehensive Aging Strategy
Metabolic interventions:
- Ketones (MCT oil, exogenous ketones, ketogenic diet)
- Intermittent fasting (16:8 minimum)
- Exercise (Zone 2 cardio + resistance training)
- Sleep (7-9 hours, address apnea)
Electrophysiological interventions:
- IAF neurofeedback (if IAF <9.5 Hz)
- Theta/beta ratio training (if ADHD-like symptoms)
- Alpha asymmetry (if depression/low motivation)
Monitoring:
- QEEG baseline at age 40-45
- Re-assess every 3-5 years
- If IAF drops <9 Hz, intensify interventions
Your brain's electrical activity reflects its metabolic state. Slowing brain waves = energy crisis. Training them back up + providing better fuel = comprehensive neuroprotection.
Conclusion: Your Brain's Metabolic Future Starts Today
If you're 44 or older, your brain is already experiencing metabolic stress. The networks are destabilizing. But if you're under 60, neurons are still viable—stressed, but salvageable.
The window is closing.
Once vascular damage accumulates and neurons die, intervention becomes far less effective. By 70, you're managing decline, not preventing it.
The interventions are accessible:
- Intermittent fasting (free)
- Exercise (free)
- Mediterranean diet (inexpensive)
- Sleep optimization (free)
You don't need expensive supplements or experimental treatments. The science supports simple metabolic strategies—if you start early.
The real question isn't "Will this work?"
The evidence is strong. The question is: Will you start now, or wait until symptoms force you to?
Age 44 is a biological reality, not a calendar event. Your brain doesn't care about your chronological age—it cares about metabolic health.
Don't wait for memory problems. Start supporting your brain's metabolism today, while neurons are still listening.
TAGS
Related Articles
SMR Neurofeedback: Train Sleep, Focus, and Self-Control
SMR (sensorimotor rhythm, ~12–15 Hz) is the workhorse protocol in neurofeedback: it builds calm alertness, improves sleep spindles, and stabilizes impulse control by strengthening thalamocortical inhibition.
Why Does My ADHD Kid Make Me Yell? (And What to Do About It)
You asked your child to put on their shoes fifteen minutes ago. They're still sitting on the floor, one shoe on, building a Lego tower, completely oblivious to the fact that you're late for school.
Brain Biohacking with Photobiomodulation (Red Light)
Photobiomodulation uses specific light wavelengths to enhance mitochondrial function and support neuroplasticity. Review the evidence for red and near-infrared light therapy.
About Dr. Andrew Hill
Dr. Andrew Hill is a neuroscientist and pioneer in the field of brain optimization. With decades of experience in neurofeedback and cognitive enhancement, he bridges cutting-edge research with practical applications for peak performance.
Get Brain Coaching from Dr. Hill →