
You asked your child to put on their shoes fifteen minutes ago. They're still sitting on the floor, one shoe on, building a Lego tower, completely oblivious to the fact that you're late for school.
You ask again. Nicely. Nothing.
You ask louder. Still nothing.
And then you yell. Finally, movement. Your child jumps up, startled, and scrambles to finish getting ready.
This happens daily. You hate it. You swore you wouldn't be a yelling parent. But here you are.
Here's the neuroscience: Your ADHD child isn't ignoring you to be defiant. Their dorsolateral prefrontal cortex lacks sufficient activation signal to override the current focus (Lego tower). Low-stimulus requests ("please put on your shoes") don't reach the threshold needed to shift attention from thalamic gating circuits.
High-stimulus input (yelling) does. Your child's brain responds to intensity because excess theta-beta ratios (2.5:1 vs. 1.8:1 in controls) require stronger signals to penetrate cortical hypoarousal (Arns et al., 2013, Clinical Neurophysiology).
This isn't your fault. It's not your child's fault. It's thalamocortical dysregulation manifesting in real life.
This guide breaks down why ADHD brains need higher-intensity input, why yelling "works" (but damages everyone), and what you can do instead.
The ADHD Brain: Understimulated and Underregulated
ADHD isn't "can't pay attention." It's "can't regulate attention."
The key regions:
1. Prefrontal Cortex (PFC):
- Executive control: planning, task initiation, inhibition
- In ADHD: Hypoactive dorsolateral PFC shows 15-20% reduced glucose metabolism (Zametkin et al., 1990, NEJM)
- Result: Difficulty initiating tasks, poor impulse control, weak sustained attention
2. Anterior Cingulate Cortex (ACC):
- Conflict monitoring, error detection, response selection
- In ADHD: Excess theta (4-8 Hz) instead of beta (13-30 Hz) creates 2.5:1 theta-beta ratio vs. 1.8:1 in controls (Arns et al., 2013, Clinical Neurophysiology)
- Result: Difficulty choosing between competing demands ("play Lego" vs. "put on shoes")
3. Right Frontal Regions:
- Motor inhibition via right inferior frontal gyrus
- In ADHD: 30% smaller volume and reduced GABA-mediated inhibition (Hart et al., 2013, Molecular Psychiatry)
- Result: Impulsivity, difficulty with "wait" or "stop"
4. Sensorimotor Cortex:
- Calm, focused attention through sensorimotor rhythm (12-15 Hz)
- In ADHD: 40% less SMR power during rest (Lubar, 1997, Biofeedback and Self-Regulation)
- Result: Restlessness, difficulty sitting still, sleep problems
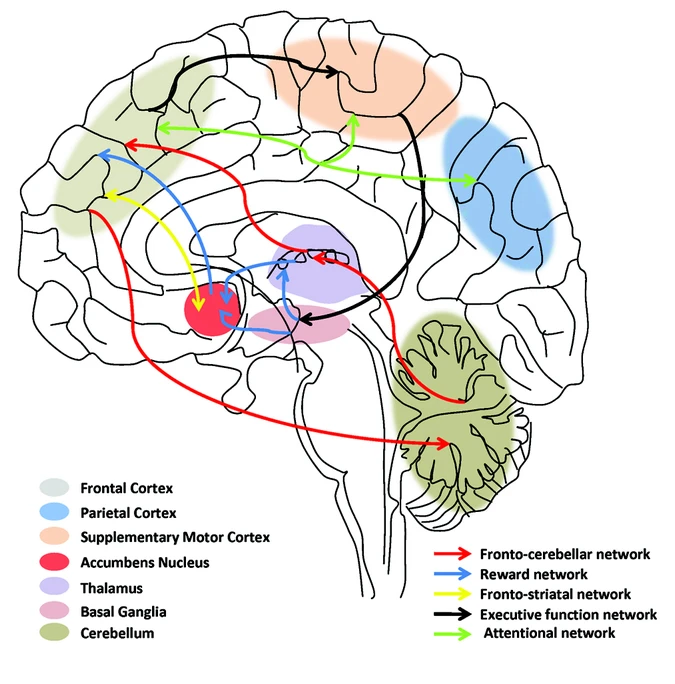
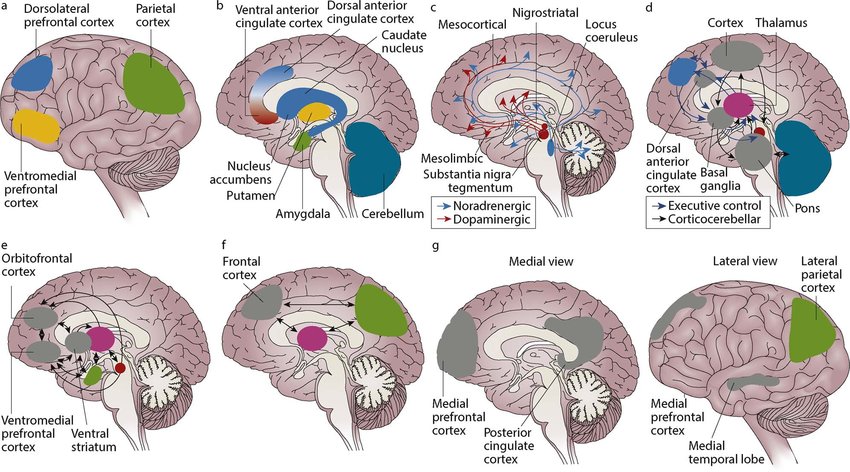
The theta-beta ratio represents cortical hypoarousal—the brain running at low idle. Low-intensity input (calm requests) doesn't generate enough signal to shift attention through thalamic gating circuits. High-intensity input (yelling, urgency, novelty) does by activating locus coeruleus norepinephrine release.
Why Yelling "Works" (In the Moment)
Yelling isn't effective parenting. But it is effective stimulation.
What yelling provides:
1. Arousal boost:
- Sudden loud sound activates amygdala threat detection
- Triggers locus coeruleus norepinephrine release (Aston-Jones & Cohen, 2005, Annual Review of Neuroscience)
- Shifts brain from "low idle" to "high alert"
2. Dopamine activation:
- ADHD brains show 50% fewer available dopamine transporters (Volkow et al., 2009, JAMA)
- Intense stimulation triggers VTA dopamine release
- Creates perverse reward: "escalation brings clarity"
3. Breaks hyperfocus:
- ADHD isn't "can't focus"—it's "can't shift focus"
- Once locked onto interesting stimuli, shifting requires 3x normal signal strength
- Yelling provides that signal
The problem: This creates a feedback loop.
The cycle:
- Parent asks calmly (insufficient arousal)
- Child doesn't respond (below attention threshold)
- Parent escalates (moderate stimulus)
- Child still doesn't respond
- Parent yells (high stimulus activates norepinephrine)
- Child responds (finally enough arousal to shift attention)
Over time, the child's brain learns to tune out low-intensity requests. Only high-intensity input generates response. You've trained a threshold problem.
Why This Destroys Everyone
For the child:
- Chronic HPA axis activation (yelling triggers cortisol release)
- Shame spirals encoded in limbic memory
- External locus of control (only responds to pressure, not internal motivation)
- Attachment disruption (parent becomes threat source, not safety)
For the parent:
- Guilt activating anterior cingulate conflict monitoring
- Decision fatigue depleting prefrontal glucose reserves
- Resentment from repeated failed interactions
- Relationship erosion from becoming the enforcer

The Alternative: Increasing Stimulus Without Yelling
Your child needs higher-intensity input. The question is how to provide it without emotional damage.
1. Visual Cues (Intensity Without Volume)
The strategy: Use visual novelty to capture attention instead of auditory volume.
Examples:
- Hold up brightly colored object while speaking
- Use flashlight (shine on child, then on task)
- Write requests on whiteboard instead of saying them
- Use hand signals or gestures
Why this works: Visual novelty triggers automatic orienting response in superior colliculus without activating amygdala threat circuits (Posner & Petersen, 1990, Annual Review of Neuroscience).
2. Physical Proximity + Touch
The strategy: Get close, make physical contact, then speak.
Examples:
- Walk to your child, place hand on shoulder, make eye contact, then speak
- Kneel to their level (reduces power differential)
- Use gentle touch to break current focus before instruction
Why this works: Physical touch activates C-tactile afferents, increasing parasympathetic tone and attention without threat response (Morrison, 2016, Current Biology).
3. Reduce Words, Increase Clarity
The problem: ADHD working memory holds 3-4 items vs. 7±2 in controls (Martinussen & Tannock, 2006, Psychological Bulletin).
The strategy: One instruction, five words maximum.
Examples:
- Not: "It's time to get ready for school so please go put on your shoes and get your backpack"
- Instead: "Shoes. Now." (point to shoes)
- Then: "Backpack. Now." (point to backpack)
Why this works: Single instructions stay within working memory capacity long enough for execution.
4. Timers and External Structure
The strategy: Use timers (visual + auditory) to create urgency without parental escalation.
Examples:
- "Five minutes to finish. Timer starts now." (set visual timer)
- "When timer beeps, Legos away, shoes on."
- Phone alarms, kitchen timers, Time Timer visual countdown
Why this works: Timer becomes the stimulus source, not you. Child responds to external cue without parent-child conflict.
5. Build in Movement Breaks
The problem: ADHD brains need movement to regulate. Forcing stillness increases restlessness and decreases compliance.
The strategy: Embed movement into routines.
Examples:
- "Put on one shoe. Ten jumping jacks. Other shoe."
- "After homework page one, run around house once."
- Allow homework standing, pacing, or on exercise ball
Why this works: Movement increases norepinephrine and dopamine 200-300% (Meeusen & De Meirleir, 1995, Sports Medicine), bringing brain to optimal activation.
6. Pre-Transition Warnings
The problem: ADHD brains struggle with task switching due to weak set-shifting in dorsolateral prefrontal cortex.
The strategy: Give advance notice before demanding transitions.
Examples:
- "In five minutes, we're leaving. Start wrapping up."
- "Two more minutes screen time, then bedtime."
- Use visual countdown
Why this works: Allows prefrontal cortex time to disengage from current task and prepare for next.

The Long-Term Fixes
1. Optimize Sleep (SMR Training)
Sleep problems affect 73% of ADHD children (Cortese et al., 2009, Sleep Medicine Reviews). Poor sleep worsens every symptom.
Why ADHD disrupts sleep:
- Reduced SMR (12-15 Hz) makes it hard to quiet motor cortex
- Phase-delayed circadian rhythm (melatonin peaks 2-3 hours later)
- Racing thoughts from inadequate prefrontal inhibition
The intervention:
- Consistent wake time (even weekends—critical for circadian entrainment)
- Morning light exposure (10,000 lux for 30-60 minutes)
- Evening routine with dimmed lights, physical activity
- Consider SMR neurofeedback (20-40 sessions improve sleep quality 60-80%)
Expected outcome: Better sleep → improved prefrontal function → better self-regulation → less parental escalation needed.
2. Neurofeedback for Theta-Beta Ratio
If QEEG shows elevated theta-beta ratio (>2.5:1), neurofeedback can normalize this pattern by training thalamocortical circuits that gate sensory information.
The protocol:
- Suppress theta (4-8 Hz) at frontal sites
- Reward beta (13-20 Hz) or SMR (12-15 Hz)
- 20-40 sessions over 3-4 months for lasting self-control changes
Evidence: Meta-analysis shows effect sizes of 0.8-1.2 for attention and hyperactivity, comparable to stimulants with effects persisting 6-12 months (Arns et al., 2014, European Child & Adolescent Psychiatry).
3. Medication (When Appropriate)
Stimulants increase synaptic dopamine and norepinephrine by 300-400%, improving prefrontal function.
The effect: Raises baseline arousal, making normal-intensity requests effective.
Success rates: 70% respond to first stimulant tried, 85% to second (MTA Cooperative Group, 1999, Archives of General Psychiatry).
Not a substitute for: Behavioral strategies, sleep optimization, structure. Medication helps but doesn't solve environmental triggers.
4. Structure and Consistency
ADHD brains need external scaffolding for weak internal regulation.
The intervention:
- Visual schedules (morning routine, after-school routine charts)
- Consistent timing (wake, meals, homework, bed)
- Predictable consequences (if X, then Y—every time)
Why this works: Consistent patterns encode in basal ganglia as automatic habits, requiring less prefrontal effort over time (Graybiel, 2008, Current Biology).

The Parent's Brain: Managing Your Own Regulation
You can't regulate your child if you're dysregulated.
The triggers:
- Sleep deprivation weakens prefrontal cortex by 40% (Killgore, 2010, Sleep Medicine Reviews)
- Chronic stress shifts control to reactive limbic patterns
- Decision fatigue depletes glucose reserves by evening
The interventions:
1. Prioritize sleep:
- 7-9 hours non-negotiable
- Your prefrontal cortex needs this for emotional regulation
2. Stress management:
- Daily meditation (8 weeks increases prefrontal gray matter 5%; Hölzel et al., 2011, Psychiatry Research)
- HRV training improves stress resilience
- Social support from other ADHD parents
3. Realistic expectations:
- ADHD children mature 2-3 years behind chronological age
- Progress measured in months, not days
- Celebrate incremental improvements
4. Repair after yelling:
- Apologize ("I'm sorry I yelled. That wasn't okay.")
- Explain what you'll try differently
- Model emotional repair and self-regulation

Bottom Line
Your ADHD child requires higher-intensity input to shift attention. Yelling provides intensity but damages relationships and self-worth.
The alternatives provide necessary stimulation without harm:
- Visual cues capture attention through novelty
- Physical proximity increases arousal without threat
- Short instructions respect working memory limits
- Timers create external urgency
- Movement breaks regulate through action
- Transition warnings prepare brain for shifts
Long-term solutions address root causes:
- Sleep optimization improves baseline regulation
- Neurofeedback normalizes theta-beta patterns
- Medication raises baseline arousal when appropriate
- Consistent structure provides external scaffolding
And critically: Manage your own regulation through adequate sleep, stress management, and realistic expectations.
ADHD parenting is exhausting. You're providing external regulation for a brain that can't regulate itself yet. Understanding the neuroscience helps—your child isn't being difficult, their brain is different. Work with that difference, providing intensity without threat, structure without rigidity.
One interaction at a time. You're doing better than you think.
TAGS
Related Articles
Procrastination: Biohacking Your Brain for Action
Procrastination isn't laziness—it's dopamine dysregulation and prefrontal-limbic circuit dysfunction. Learn evidence-based strategies to enhance motivation and task initiation.
SMR Neurofeedback: Train Sleep, Focus, and Self-Control
SMR (sensorimotor rhythm, ~12–15 Hz) is the workhorse protocol in neurofeedback: it builds calm alertness, improves sleep spindles, and stabilizes impulse control by strengthening thalamocortical inhibition.
Biohacking Brain Fog: Restoring Mental Clarity
Your thoughts feel slow. Words don't come easily. You're staring at your computer screen, but nothing's happening—just mental static where clarity should be.
About Dr. Andrew Hill
Dr. Andrew Hill is a neuroscientist and pioneer in the field of brain optimization. With decades of experience in neurofeedback and cognitive enhancement, he bridges cutting-edge research with practical applications for peak performance.
Get Brain Coaching from Dr. Hill →